Peaceful Pill Blog

Overcoming Impediments to MAiD Another approach?
Overcoming impediments to medically assisted dying: A signal for another approach? This Blog was originally published in the British Medical Journal of Medical Ethics on 6 April 2023. By Juergen Dankwort (Chapter Coordinator - Canada, Exit International) The proposal to provide assistance with voluntary assisted dying (VAD) has grown significantly ...
Read More
Read More
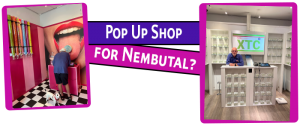
What if there were a Shop for Nembutal?
Over summer, Exit's Philip Nitschke made the trek to the Dutch city of Utrecht to have a look at the new XTC (ecstasy) pop-up shop, asking what if there were a Shop for Nembutal? An initiative of the Poppi Drug Museum in Amsterdam and in partnership with the University of ...
Read More
Read More

Backlog of Euthanasia Requests by Mental Health Sufferers
In a report to the Dutch Parliament this week, the Dutch Minister for Health, Ernst Kuipers, has reported on the problems associated with the backlog of euthanasia requests by mental health sufferers (inc those with dementia) in the Netherlands. Reports such as this are a key element in the Netherland's ...
Read More
Read More

Pros & Cons of Couples Going Together
The Pros & Cons of Couples Going Together is a topic that needs comment, especially in light of the recent alleged botched double suicide of Exit Members Marijke and Tony Smyth in Queensland in Australia. By Fiona Stewart I want to compare this awful ordeal (at least as it was ...
Read More
Read More

Be careful who you tell
Be careful who you tell is the message from Exit's long-time Melbourne Chapter Coordinator, Chris Lovelock. After long and careful consideration and forethought Chris had made an Exit Plan. Chris told a 'close friend' about this plan. Unfortunately, the so-called 'close friend' then told the Police. Here is what happened ...
Read More
Read More
Legalising assisted suicide is a slippery slope says Dr Anthony Latham
Legalising assisted suicide is a slippery slope says Dr Anthony Latham in the Scotsman. Not so fast says Exit! When an opinion piece appears in the right to life press, my tendency is usually to dismiss it. Because it is written for a specific, one-eyed readership, it is to be ...
Read More
Read More
The Swiss Option Just Got Harder
The Swiss Option Just Got Harder in what some say is a veiled attempt to stop foreigners having a VAD in Switzerland. This week the Swiss Medical Association (SAMS) tightened its grip over when and how Swiss doctors can provide assisted suicide. While, from a legal point of view, anyone ...
Read More
Read More

Cancel Culture gets Uncancelled with Podcast Published
In January 2022 Exit Director Philip Nitschke was contacted by the 'Let's Get Psyched' radio show and podcast series which is hosted by a group of psychiatrists/ psychologists at the University of California, Riverside with an invitation to take part in their program. Let's Get Psyched wrote: 'The hosts at ...
Read More
Read More
Fudging the Facts in the Azide Wars
This week in Fudging the Facts in the Azide Wars, my old colleague, psychiatrist Boudewijn Chabot wrote a prominent opinion piece in the Dutch newspaper NRC called 'I can't warn enough about Middel X'. Normally, I would welcome an opinion from a fellow activist, but not this week. Chabot's column ...
Read More
Read More
Ensuring Northern Territory Rights Bill 2021
The below is the submission of Exit International to the Australian Senate inquiry into the current ban on the Northern Territory making laws on assisted suicide/ voluntary euthanasia, 30 August 2021. Committee Secretary Senate Legal and Constitutional Affairs Committee PO Box 6100 Parliament House Canberra ACT 2600 29 August 2021 ...
Read More
Read More
Exit